8 Common Myths on Hormone Replacement Therapy (HRT)
Read the most common misconceptions now and start treatment early. Let me start with the top two that drive me crazy.
One – “It’s just menopause and you need to get used to it.”
Or “Menopause is a normal part of life,” or “This is your new normal and you just need to learn to live with it”. False. Pardon me for a moment while I vent, but are men with erectile dysfunction being told that it’s a normal part of life and they should just get used to it? Heck no! They are given the fastest prescription for Viagra and out the door they go, or rather skipping down the sidewalk beside the white picket fence (recall the 2002 commercial). Meanwhile, us ladies are sitting in the doctor’s office begging for someone to just listen, maybe validate our concerns, or maybe, just maybe, provide some helpful medical advice? But that’s not the reality. In 2022, researchers from Yale University looked at over 500,000 insurance claims of women seeking healthcare for various stages of perimenopause. They found 300,000 claims were related to
- Women seeking medical assistance for their menopause related symptoms AND
- that 75% left their medical appointments without any treatment for their concerns.
Wow. My point is – if you’re not getting the help you need – go elsewhere.
Two – You must be 12 months without a period to qualify for HRT
False. There is no need to suffer! A woman can be suspended in perpetual peri-menopause for 1 to 5 to 7 years as symptoms increase while your health declines. To be clear, the 12 months without a period is what defines official menopause, but it should not define your candidacy for HRT. A skilled doctor will be able to guide you in stepwise order on which hormones are appropriate, in what form and at what doses, early during your transition.
Three – You can’t take HRT if you have had endometriosis
False. You are not excluded from HRT if you’ve had a history of endometriosis. Rather, it is important to ensure progesterone is on board for protection of the uterus. Again, a skilled doctor who is trained in HRT will be able to guide you.
Four – A history of adenomyosis automatically excludes you from HRT.
False. Adenomyosis is a condition where the tissue that normally lines the uterus, called the endometrium, grows into the muscular wall of the uterus (the myometrium). This requires some caution and emphasis on the need to always have progesterone on board as well.
Five – A family history of heart disease, liver disease or breast cancer automatically excludes you from HRT.
False – the latest research and expert consensus challenge the notion that a family history alone should disqualify a woman from HRT candidacy.
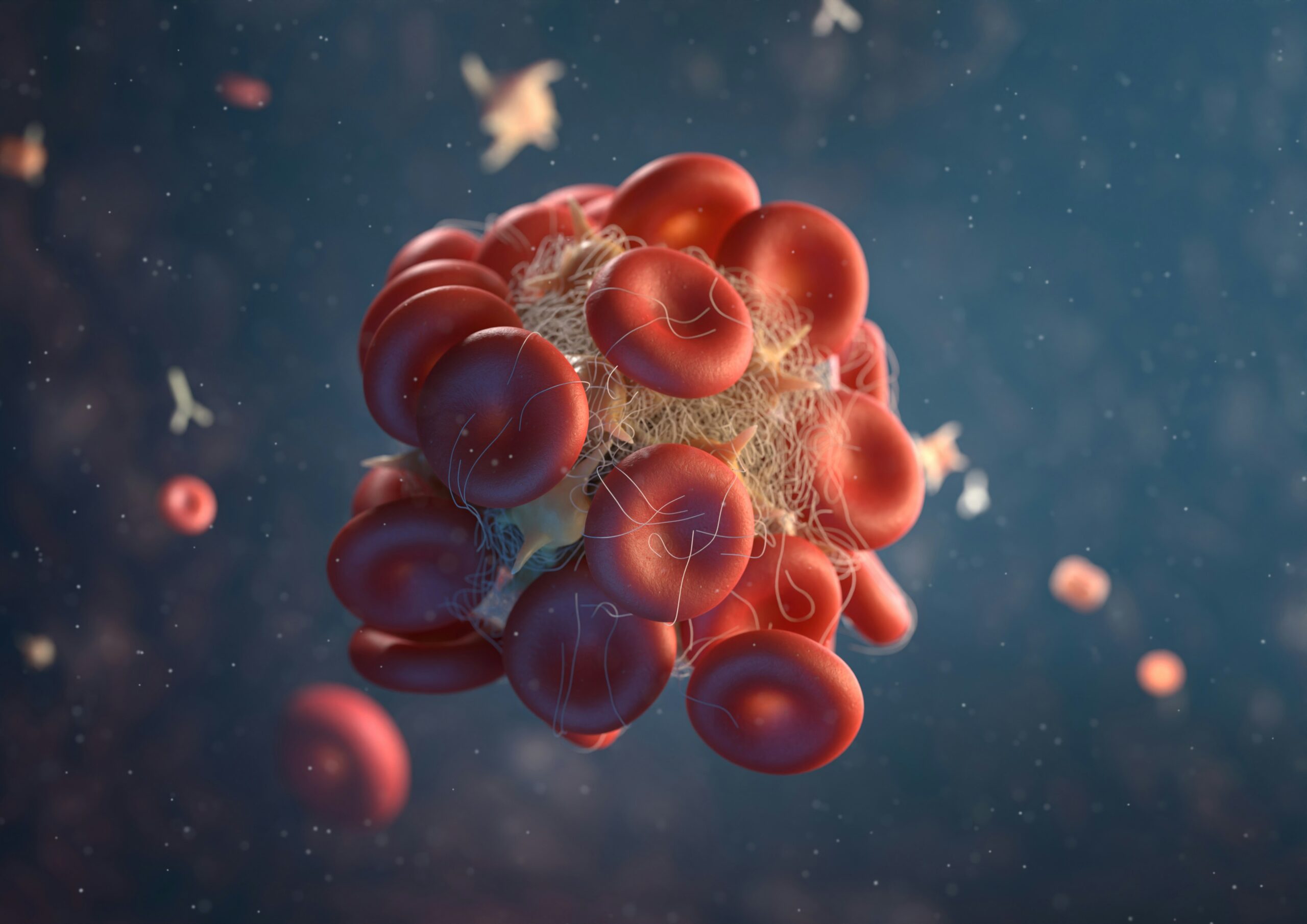
Six – Concerns over an increased risk of clotting should automatically exclude you from HRT
False. There’s a difference between venous blood clots (DVT and pulmonary embolism) versus arteriolar clotting. In the WHI clinical trials, there was no increase in risk in Arteriolar clotting seen in women who started HRT within the 10-year window following the onset of the last menstrual bleed. Non oral formulations of HRT … do not increase the risk!
Seven – A history of migraine headaches automatically excludes you from HRT
False! There is no increased risk of stroke in women who have migraine headaches without auras. If a woman has a history of migraine with Aura – both the CDC and the WHO guidelines recommend these women do not use combined hormone contraception – due to the very slight but present increased risk of stroke – especially in women who smoke. A similar contraindication has not been identified in those women with migraines who need HRT for menopausal symptoms – as the doses for HRT are much smaller and much lower for HRT than those in oral contraceptive pills.
Eight – You should never use HRT if you had breast cancer.
False. Talk to a doctor who understands the evidence. Having had and overcome cancer is a special circumstance that comes with surgery, chemotherapy and/or radiation and even more special insults to your body. The consideration for HRT is not a hard no – rather, the correct form and dose can help alleviate the uncomfortable side effects of cancer treatments and prevent the real risk of recurrence, rather than be the cause. This is important, highly controversial and deserves some clarification and a deeper conversation with your physician – one who is trained in HRT.
Read more on the benefits of HRT.
If hormone replacement therapy was so dangerous, as some tout it to be, why then is the BC provincial government – the first across the country – now funding hormone replacement therapy (HRT)? Because – our government has reviewed the research and recognizes that women going through menopause deserve to be supported.
Written by Dr. Emina Jasarevic, ND